The Critical Truth About Fibromyalgia: Is It a Life-Altering Illness or Just Chronic Discomfort?
Fibromyalgia has long been a subject of misunderstanding and misdiagnosis. Often dismissed as a vague or exaggerated complaint, this chronic condition is now gaining recognition for the serious impact it can have on a person’s daily life. The focus keyword “Is fibromyalgia a critical illness?” triggers a crucial inquiry—how serious is this condition, medically and legally?
Understanding the Nature of Fibromyalgia
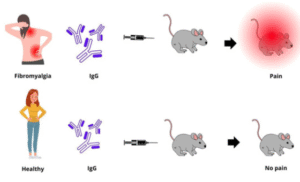
Fibromyalgia is a chronic disorder known for widespread musculoskeletal pain accompanied by fatigue, sleep problems, memory issues, and mood disturbances. The condition affects the way the brain and spinal cord process pain signals, leading to amplified pain sensations even without direct cause.
Unlike acute illnesses, fibromyalgia doesn’t come on suddenly or resolve quickly. It’s persistent, often lifelong, and requires comprehensive lifestyle adjustments. However, because it doesn’t damage organs or shorten lifespan, it falls into a grey area when determining whether it qualifies as a “critical illness.”
Medical Classification: Is It Critical?
In a clinical context, a critical illness is generally defined as a condition that poses a serious threat to life or significantly impairs bodily function. Conditions like cancer, stroke, or heart disease are often listed under this category.
By that definition, fibromyalgia may not be considered a traditional critical illness because it doesn’t cause tissue damage, permanent disability, or death. However, its chronic nature and the severe pain and fatigue it causes can be profoundly disabling.
Some physicians and researchers argue that fibromyalgia should be recognized as a critical illness due to its impact on quality of life. Patients often experience depression, anxiety, reduced physical activity, and an inability to work, which can result in economic hardship and social isolation.
Insurance Industry Perspective
From an insurance standpoint, critical illness coverage typically includes illnesses that have high mortality or require intensive medical intervention. Fibromyalgia is rarely included in such policies unless it results in total disability or is linked to another covered condition.
This exclusion creates a dilemma for those living with fibromyalgia. They may face high medical expenses, reduced earning capacity, and significant lifestyle changes without the financial support that comes with a critical illness designation. For disability insurance claims, fibromyalgia is more likely to be considered if sufficient medical documentation and functional assessments are provided.
Functional Impairment and Work Limitations
Fibromyalgia can lead to significant functional impairments. Chronic pain, sleep disruption, and cognitive difficulties (often called “fibro fog”) interfere with work performance, especially in physically demanding or high-stress jobs.
Some patients are forced to transition to part-time work, seek disability accommodations, or stop working altogether. The inability to maintain employment over time positions fibromyalgia closer to the practical definition of a critical illness in terms of life disruption.
Legal and Social Recognition
Different countries and regions recognize fibromyalgia in varying ways. In some jurisdictions, it is considered a legitimate basis for receiving disability benefits, particularly when symptoms are severe and well-documented. In others, it remains contested, with individuals needing extensive proof of their limitations to qualify for support.
The social perception of fibromyalgia also influences its status. Because symptoms are invisible and not always measurable through standard tests, sufferers often encounter skepticism from employers, insurers, and even family members. This lack of validation adds an emotional burden to an already challenging condition.
Living with Fibromyalgia: A Day-to-Day Challenge
Managing fibromyalgia involves more than just treating pain. Patients must adopt a comprehensive lifestyle strategy that includes physical therapy, stress management, adequate sleep, and often medication. Despite these efforts, symptom flares can still occur without warning, disrupting routines and diminishing personal independence.
This level of ongoing management and the unpredictability of the illness contribute to the argument that fibromyalgia should be regarded as a serious, if not formally critical, condition.
Final Thoughts
So, is fibromyalgia a critical illness? From a strictly medical or insurance perspective, it may not meet the traditional criteria. However, when viewed through the lens of daily function, emotional well-being, and long-term quality of life, fibromyalgia can be every bit as life-altering as conditions labeled “critical.”
Understanding fibromyalgia in its full context—biological, psychological, social, and economic—is essential. Only then can healthcare systems, insurers, and society at large begin to give this condition the recognition and support it demands.